Why Air Pollution Matters More Than You Think
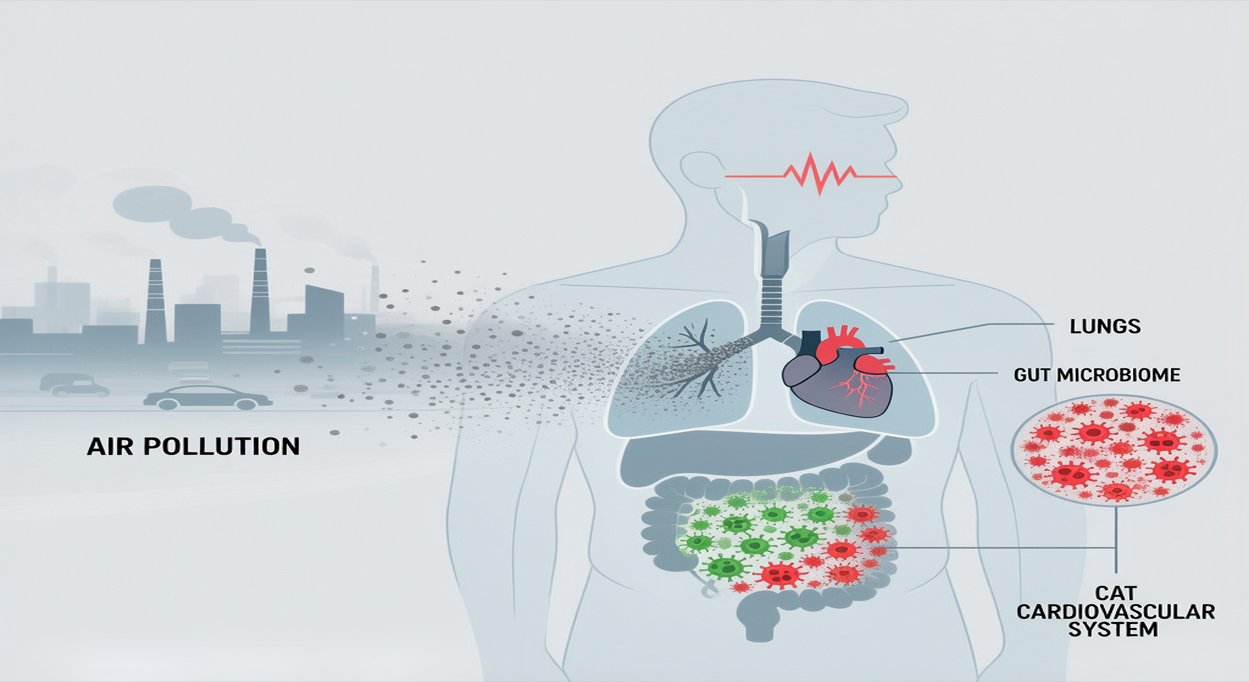
Let’s be honest—air pollution isn’t just some distant problem. Pretty much everyone on the planet breathes in dirty air every single day. That’s not an exaggeration. Around 99% of us are stuck with air that’s way above the recommended safety limits. We’re talking about stuff like tiny particles, nitrogen oxides, ozone, and other chemicals floating around. They don’t just hang out in the air; they slip right into your lungs and even make their way into your bloodstream.
The health risks? They’re downright shocking. Air pollution kills over three million people every year. That’s more than diabetes, smoking, or obesity. What’s wild is how many people just don’t realize what this does to their bodies. Breathing polluted air day in and day out quietly damages your organs, even if you don’t feel it right away.
So, what’s actually in this stuff? The worst offenders are things like particulate matter—basically, tiny bits of dust and dirt. The really fine particles (PM2.5) and slightly bigger ones (PM10) are especially bad because they’re small enough to dodge your body’s natural defenses. They dig deep into your lungs, sneak past barriers, and end up circulating throughout your body. And that’s where the real trouble starts
Air pollution isn’t just about particulate matter. There’s nitrogen dioxide (NO₂), ozone (O₃), sulfur dioxide (SO₂), and a whole mix of volatile organic compounds (VOCs) floating around too. All of these can trigger inflammation in your lungs, mess with your body’s defenses, and set off reactions that ripple throughout your system.
The Gut-Lung Axis: How Air Pollution Gets to Your Gut
So, how does dirty air end up messing with your gut? It’s actually a bit of a journey. When you breathe in polluted air, some particles settle in your airways. Your body tries to fight back—tiny hairs and mucus work together, sweeping those particles up toward your throat. You swallow, and just like that, the stuff you breathed in ends up in your digestive tract along with saliva and mucus.
But that’s not the whole story. Some of the smallest particles can slip right through the lining of your lungs, pass into your bloodstream, and travel all over your body—including your gut. So, you’ve got two main routes: you swallow some pollution, and some just rides along in your blood. That’s why air pollution hits your gut health so hard.
The Gut Microbiota and What It Does
Your gut is home to trillions of microbes—bacteria that handle all kinds of jobs your body needs. They make vitamins, break down nutrients, fight off harmful germs, and help train your immune system. When your gut’s microbial community is balanced and diverse, it keeps your intestinal lining strong and your metabolism and immune system on track. This balance is key for your health.
Your gut is home to trillions of bacteria, mostly from two main groups: Firmicutes and Bacteroidetes. There’s also a smaller crowd of helpful microbes like Verrucomicrobia. When everything’s in balance—what scientists call eubiosis—your gut and these microbes live together in a partnership that’s been evolving for millions of years.
But then air pollution comes in and throws everything off. Studies show that breathing in polluted air changes your gut bacteria in a big way. Tiny particles like PM2.5 and PM10 don’t just lower the overall variety of microbes (which is bad news for gut health), they also let the troublemakers—bacteria like Proteobacteria and Deferribacterota—take over. At the same time, the good guys like Verrucomicrobia start to disappear.
So how does this happen? Air pollutants hit the gut lining and trigger oxidative stress, kicking off a burst of reactive oxygen species (ROS). These ROS damage bacteria and mess up the chemical environment they need to thrive. On top of that, pollution activates certain immune receptors and sets off both local and whole-body inflammation, which just makes the whole situation worse.
One of the scariest things about this disruption is what it does to your gut barrier. Normally, a thick mucus layer and tight junctions between cells keep harmful stuff out of your bloodstream. But when pollution upsets the microbial community, that barrier gets weaker. The mucus thins out, and those tight junctions start to fail. Suddenly, bacteria and their toxic bits (like lipopolysaccharides, or LPS) slip through the cracks and end up in your blood.
This “leaky gut” problem sparks full-body inflammation. Bacterial products in the bloodstream push immune cells into overdrive, raising levels of inflammatory markers such as TNF-alpha and interleukins. That constant inflammation isn’t just uncomfortable—it’s a key reason why air pollution is tied to heart disease.
And this isn’t just theory. Big studies back it up. The MESA Air study, for example, found that people living in cities with higher PM2.5 levels had faster buildup of calcium in their heart arteries—an early sign of heart disease. Another study, the Aragon Workers Health Study, linked exposure to metals like arsenic, cadmium, and titanium in air pollution directly to the development of artery-clogging plaque, even before symptoms show up.
So, the link is clear: air pollution messes with your gut, weakens your defenses, and sets off inflammation that can damage your heart.
Acute effects are just as alarming. In Spain, the Codi IAM registry tracked a clear spike in daily hospital admissions for ST-elevation myocardial infarctions (STEMIs), life-threatening heart rhythms, and deaths right after short bursts of high PM2.5 and PM10 pollution. So, even a few hours or days of breathing dirty air can set off serious heart problems, especially in people who are already at risk.
How Air Pollution Hurts the Heart
Air pollution attacks the heart through several tangled pathways. When you breathe in fine particles, your lungs take the first hit. The particles spark inflammation, releasing a flood of cytokines and oxidative stress molecules. These troublemakers don’t stay put. They spread through the blood, damaging the endothelium—the thin lining inside your blood vessels. Once that lining’s in trouble, blood vessels don’t relax or seal themselves as they should.
There’s another important angle here—the gut. Air pollution can throw the gut’s bacterial community way off balance. This “dysbiosis” means more bacterial toxins like lipopolysaccharides leak into your bloodstream, while the gut stops making enough helpful short-chain fatty acids. The end result? Chronic inflammation ramps up, which speeds up plaque buildup in arteries, makes those plaques less stable, and raises the chances of blood clots.
Pollution also pushes up blood pressure. It does this by cranking up the sympathetic nervous system and messing with blood vessel function. Over time, people exposed to more fine particles (PM2.5) tend to develop high blood pressure, which is a huge risk factor for heart disease all on its own.
Metabolic Consequences: Obesity, Diabetes, and More
The Gut, Pollution, and Metabolic Disease
It’s not just the heart. Air pollution’s effect on the gut raises the risk for obesity and type 2 diabetes, too. Studies in overweight teens who live with heavy traffic pollution show a direct link: the more pollution, the higher their fasting blood sugar. Their gut bacteria also shift toward types known to fuel insulin resistance, like Bacteroidaceae and Coriobacteriaceae.
Digging deeper, researchers found that changes in gut bacteria explained about a quarter of the connection between air pollution and higher blood sugar. So, the gut microbiome isn’t just caught in the crossfire—it’s a key part of the chain reaction that leads from pollution to metabolic disease.
Short-Chain Fatty Acids and the Leaky Gut Problem
Normally, a healthy gut microbiome cranks out short-chain fatty acids (SCFAs), especially butyrate, which help keep the gut wall strong and the immune system in check. Butyrate, made mainly by Faecalibacterium and other Firmicutes, tightens up the gut’s barrier and helps suppress runaway inflammation.
When air pollution throws the gut’s balance off, SCFA production drops. The gut barrier gets weaker, making it easier for bacterial toxins to slip into the bloodstream and keep the immune system on high alert. This creates a nasty cycle—more inflammation, more dysbiosis, and a gut that just keeps getting leakier.
Vulnerable Populations and Health Disparities
Who’s at Greatest Risk?
Air pollution touches just about everyone, but some people really feel the impact more than others. Kids are especially at risk—their lungs keep growing well into their twenties, so early exposure can actually change how their microbiome develops and mess with their immune systems for life. Older adults have it tough, too. Their bodies just don’t bounce back as easily, especially if they already have heart problems or other health issues.
People dealing with existing conditions—like obesity, diabetes, heart disease, or asthma—take an even bigger hit from air pollution. And if you live in a low or middle-income country, the odds are stacked higher. Folks there often breathe in more pollution and, at the same time, struggle to get proper healthcare. That gap leads to some pretty stark health inequalities.
Pregnancy and Developmental Risks
Lately, research has shown some worrying links between air pollution during pregnancy and poor outcomes—things like trouble with blood sugar in pregnant women and problems at birth. These early hits can set kids up for lifelong metabolic issues, all because their microbiota gets thrown off before they’re even born.
How to Cut Down on Exposure and Protect Yourself
Personal Protective Moves
Big changes need governments and policy shifts, but you can still take steps at home. HEPA filters—those high-efficiency particulate air filters—work well in houses and cars to clear out a lot of the fine particles. With a good air purifier, you can slash PM2.5 levels inside by up to 80%.
When the air outside is bad, wearing a quality mask like an N95 or N100 helps a lot—just make sure it fits you properly and wear it consistently. Also, check your local air quality reports. If there’s an alert, try to stay indoors and skip outdoor activities until things clear up. Small choices like these really help protect your health.
Supporting Your Gut Microbiota: Everyday Choices That Matter
Cutting down on pollution exposure is one thing, but you’ve also got to look after your gut. Eating more high-fiber foods helps good bacteria thrive—they create short-chain fatty acids that keep your gut lining strong. Foods packed with probiotics, like yogurt, kefir, sauerkraut, and kimchi, can boost the variety of bacteria in your gut. The science isn’t totally settled, but these foods are worth a shot.
Moving your body regularly does more than just keep you fit—it helps your gut bacteria stay diverse and healthy, which can actually fight off some of the damage pollution does. Getting enough sleep, managing stress, and only taking antibiotics when you really need them also make a real difference for your microbiota.
Healthcare and Policy: Taking Action on a Bigger Scale
Doctors should check if patients with heart risks are exposed to a lot of pollution and talk to them about ways to protect themselves. Keeping tabs on blood pressure and heart health is even more important for people living where the air isn’t clean.
Big changes need to happen, too. Air quality programs that crack down on emissions from cars and factories, push for clean energy, and create more green spaces in cities really help protect public health. The World Bank’s Pollution Management and Environmental Health program shows that when communities get serious about cleaning up their air, fewer people get sick or die from pollution. That’s the kind of impact we need.
Emerging Research and Future Directions
Digging Deeper into Microbiota Research
It’s time to look beyond just which microbes live in our gut. Using whole-genome metagenomic sequencing, researchers can really see how air pollution changes not just the makeup, but the actual jobs these microbes do. When you pair this with fecal metabolomic profiling, you start to understand how pollution-driven changes mess with the production of important metabolites—things like short-chain fatty acids, secondary bile acids, and even the building blocks for neurotransmitters.
But there’s still a lot we don’t know. How exactly do different pollutants interact with the gut lining and the microbes themselves? Unpacking these mechanisms is key. If we nail down the details, we can start designing therapies that actually target the microbiota in a smart, focused way.
Therapies and Prevention: What’s Next?
New research points toward some promising tools—targeted probiotics, prebiotics, maybe even fecal microbiota transplants—to help people exposed to pollution. These could work alongside traditional medicine, but we need big, well-designed clinical trials to show they're really safe and effective.
Then there’s the idea of personalization. If we map out a person’s unique microbiota and figure out exactly how much pollution they’re exposed to, we can tailor treatments. This kind of precision health approach feels like where environmental health is headed.
Conclusion: Facing an Invisible Enemy
Air pollution isn’t just about coughing or asthma. It changes the way our whole body works—through the gut, through inflammation, through the heart and blood vessels. The science linking pollution to gut problems, leaky gut, and heart disease is piling up fast.
Sure, one person alone can’t clean up the air. But understanding these connections means we can make smarter choices—using air filters, paying attention to diet, maybe even working with our doctors in new ways. At the same time, governments and communities need to step up with real policies, cut emissions, and focus on sustainable solutions.
For doctors, patients, and policymakers, calling out air pollution as something we can actually change—the same way we talk about smoking or high blood pressure—matters. If we act together, mixing personal protection with big-picture policy, we can cut down on the huge health problems caused by this silent, invisible threat.







Comments
Leave a Comment
No comments yet. Be the first to share your thoughts!